Antibiotic-resistant infections to kill 39 million people by 2050 – Lancet

According to the WHO, antimicrobial resistance is one of the most pressing global public health and development threats.
Over 39 million people worldwide will die from antibiotic-resistant infections between now and 2050, according to a new Lancet report.
The report also predicts that by 2050, around two million deaths per year could be linked to drug-resistant infections.
More To Read
- Ministry warns Kenyans on escalating antibiotic resistance
- WHO sounds alarm: Antibiotic resistance rising fast, puts millions at risk worldwide
- WHO raises alarm as antibiotic resistance threatens global health gains
- Kenya's public health at risk as falsified and substandard medicines accelerate antimicrobial resistance
- Clean hands, safe bites: Why everyday food habits matter more than you think
- Senators demand urgent Ministry of Health action on child deaths from drug-resistant infections
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites evolve and resist current treatments. Key causes of AMR include the overuse and misuse of antibiotics in healthcare and agriculture, poor infection control practices in hospitals, inadequate sanitation and hygiene, and the lack of new antibiotics being developed.
In Kenya, there were 8,500 deaths directly attributable to AMR and 37,300 deaths associated with AMR in 2019.
The researchers from the Global Research on Antimicrobial Resistance Project, the Institute for Health Metrics and Evaluation, and other institutions analysed deaths and illnesses linked to AMR across 22 pathogens, 84 pathogen-drug combinations, and 11 types of infections in 204 countries and territories between 1990 and 2021. A death "attributable" to AMR is one directly caused by it, while a death "associated" with AMR may have been exacerbated by the resistance, but not necessarily caused by it.
The study found that between 1990 and 2021, AMR-related deaths decreased by more than 50 per cent in children under 5 but rose by over 80 per cent in adults aged 70 and older, a trend expected to continue.
Vulnerable adults
Dr Chris Murray, one of the study's authors, noted the surprising nature of these findings. He explained that while deaths from AMR in children have declined due to improvements in vaccination, sanitation, and treatment programmes, there has been a steady rise in deaths among older adults, who are more vulnerable to severe infections as the global population ages.
The study also highlighted methicillin-resistant staphylococcus aureus (MRSA) as the pathogen-drug combination responsible for the largest increase in AMR-related deaths, with attributable deaths nearly doubling from 57,200 in 1990 to 130,000 in 2021.
Using statistical modelling, the researchers projected that deaths linked to AMR could increase by 2050 under three scenarios: if the current situation persists, if new antibiotics are developed, or if global healthcare access improves. Without significant improvements, they estimate that by 2050, AMR could cause 1.9 million deaths directly and 8.2 million deaths indirectly.
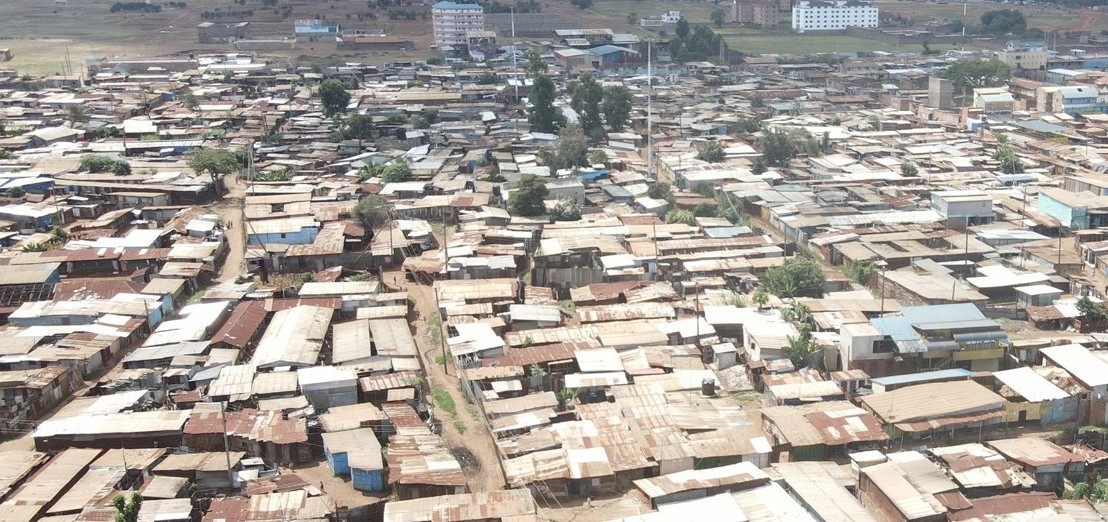
Regions such as South Asia, Latin America, the Caribbean, and sub-Saharan Africa are expected to be hit hardest, partly because many of them lack equitable access to quality health care.
Murray pointed out that in many low-resource settings, people who need antibiotics don't always have access to them, and basic care — like oxygen and intensive care units — is often unavailable. "The difference between life and death in these settings is not just about antibiotics but the whole spectrum of supportive care," he said.
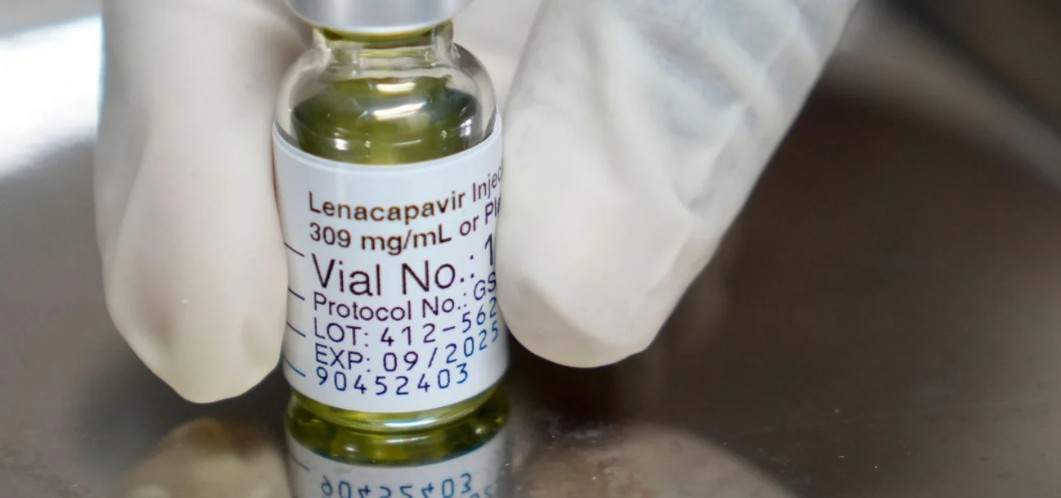
However, if global healthcare improves, the study suggests that 92 million deaths could be prevented between 2025 and 2050. If new, more powerful antibiotics are developed, around 11 million deaths could be avoided.
The study, which is based on 520 million individual records, provides a comprehensive assessment of AMR's global burden. In a commentary accompanying the study, Samuel Kariuki from the Kenya Medical Research Institute acknowledged the value of the research but cautioned that the models do not account for the emergence of new superbugs, which could lead to an underestimate of the threat.
Kariuki stressed that the data should serve as a call to action, urging investments and targeted strategies to tackle the growing problem of antimicrobial resistance worldwide.
Misuse and overuse
According to the World Health Organisation (WHO), AMR is one of the most pressing global public health and development threats. In 2019, AMR was directly responsible for an estimated 1.27 million deaths and contributed to a total of 4.95 million deaths globally. The primary drivers of AMR are the misuse and overuse of antimicrobials in humans, animals, and plants.
AMR affects countries across all income levels, but low- and middle-income countries are particularly vulnerable due to factors such as poverty, inequality, and limited access to quality healthcare. The rise of AMR threatens many of the advancements in modern medicine, as it makes infections harder to treat and increases the risks associated with essential medical procedures like surgeries, caesarean sections, and cancer treatments.
The world also faces a crisis in the antibiotics pipeline. There is a significant gap in research and development for new antibiotics, and there is an urgent need to ensure equitable access to existing and new vaccines, diagnostics, and medicines.
The economic impact of AMR is substantial. The World Bank estimates that it could result in an additional US$1 trillion in healthcare costs by 2050 and lead to annual GDP losses of between US$1 trillion and US$3.4 trillion by 2030.
To address AMR, the WHO emphasises the importance of preventing infections, ensuring universal access to quality diagnosis and appropriate treatments, and strengthening surveillance and research to support the development of novel vaccines, diagnostics, and medicines.
Top Stories Today